2022-11-29

与妊娠相关的静脉血栓栓塞是孕产妇发病率和死亡率的主要原因,有静脉血栓栓塞史的孕妇和产后妇女需要进行血栓预防。低分子肝素预防妊娠期和产后静脉血栓栓塞复发的最佳剂量是不确定的。
在2013年4月24日至2020年10月31日期间,1339名孕妇接受了符合条件的筛查,其中1110人被随机分配到体重调整的中剂量(n=555)或固定低剂量(n=555)低分子肝素组(ITT人群)。在体重调整的中剂量组555名妇女中有11人(2%)发生静脉血栓栓塞,在固定低剂量组555名妇女中有16人(3%)发生静脉血栓栓塞(相对风险[RR] 0.69[95%可信区间0.32 - 1.47];p = 0·33)。静脉血栓栓塞发生在5名(1%)中剂量组妇女和5名(1%)低剂量组妇女的产前,6名(1%)妇女和11名(2%)妇女的产后。在治疗中,安全人群(N=1045)中520名中剂量组妇女中23名(4%)发生大出血,低剂量组525名妇女中20名(4%)发生大出血(RR 1.16[95%可信区间0.65 -2·09])。
在有静脉血栓栓塞史的女性中,产前和产后联合使用体重调整的中剂量低分子肝素与固定低剂量低分子肝素相比,复发风险并不低。这些结果表明,低剂量低分子肝素用于妊娠期血栓预防是预防妊娠相关静脉血栓栓塞复发的适当剂量。
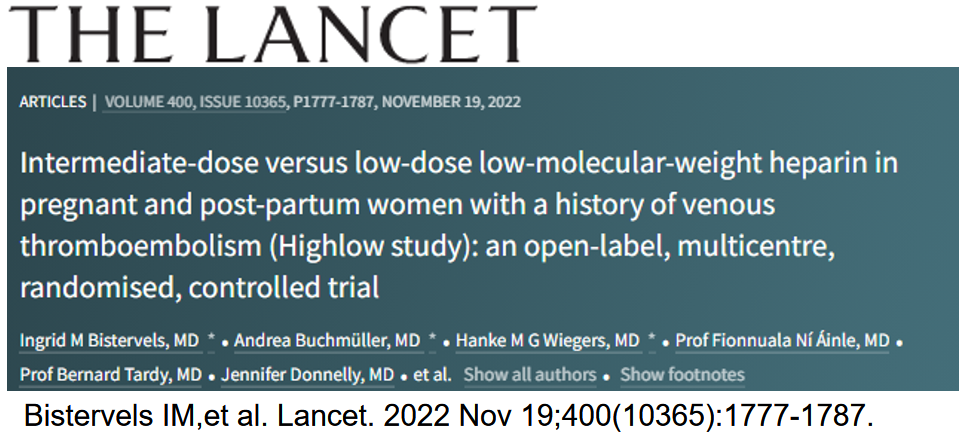
Abstract
Background: Pregnancy-related venous thromboembolism is a leading cause of maternal morbidity and mortality, and thromboprophylaxis is indicated in pregnant and post-partum women with a history of venous thromboembolism. The optimal dose of low-molecular-weight heparin to prevent recurrent venous thromboembolism in pregnancy and the post-partum period is uncertain.
Methods: In this open-label, randomised, controlled trial (Highlow), pregnant women with a history of venous thromboembolism were recruited from 70 hospitals in nine countries (the Netherlands, France, Ireland, Belgium, Norway, Denmark, Canada, the USA, and Russia). Women were eligible if they were aged 18 years or older with a history of objectively confirmed venous thromboembolism, and with a gestational age of 14 weeks or less. Eligible women were randomly assigned (1:1), before 14 weeks of gestational age, using a web-based system and permuted block randomisation (block size of six), stratified by centre, to either weight-adjusted intermediate-dose or fixed low-dose low-molecular-weight heparin subcutaneously once daily until 6 weeks post partum. The primary efficacy outcome was objectively confirmed venous thromboembolism (ie, deep-vein thrombosis, pulmonary embolism, or unusual site venous thrombosis), as determined by an independent central adjudication committee, in the intention-to-treat (ITT) population (ie, all women randomly assigned to treatment). The primary safety outcome was major bleeding which included antepartum, early post-partum (within 24 h after delivery), and late post-partum major bleeding (24 h or longer after delivery until 6 weeks post partum), assessed in all women who received at least one dose of assigned treatment and had a known end of treatment date. This study is registered with ClinicalTrials.gov, NCT01828697, and is now complete.
Findings: Between April 24, 2013, and Oct 31, 2020, 1339 pregnant women were screened for eligibility, of whom 1110 were randomly assigned to weight-adjusted intermediate-dose (n=555) or fixed low-dose (n=555) low-molecular-weight heparin (ITT population). Venous thromboembolism occurred in 11 (2%) of 555 women in the weight-adjusted intermediate-dose group and in 16 (3%) of 555 in the fixed low-dose group (relative risk [RR] 0·69 [95% CI 0·32-1·47]; p=0·33). Venous thromboembolism occurred antepartum in five (1%) women in the intermediate-dose group and in five (1%) women in the low-dose group, and post partum in six (1%) women and 11 (2%) women. On-treatment major bleeding in the safety population (N=1045) occurred in 23 (4%) of 520 women in the intermediate-dose group and in 20 (4%) of 525 in the low-dose group (RR 1·16 [95% CI 0·65-2·09]).
Interpretation: In women with a history of venous thromboembolism, weight-adjusted intermediate-dose low-molecular-weight heparin during the combined antepartum and post-partum periods was not associated with a lower risk of recurrence than fixed low-dose low-molecular-weight heparin. These results indicate that low-dose low-molecular-weight heparin for thromboprophylaxis during pregnancy is the appropriate dose for the prevention of pregnancy-related recurrent venous thromboembolism.
文章连接:
www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)02128-6/fulltext
百度浏览 来源 : 医微客
版权声明:本网站所有注明来源“医微客”的文字、图片和音视频资料,版权均属于医微客所有,非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源:”医微客”。本网所有转载文章系出于传递更多信息之目的,且明确注明来源和作者,转载仅作观点分享,版权归原作者所有。不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。 本站拥有对此声明的最终解释权。



发表评论
注册或登后即可发表评论
登录注册
全部评论(0)